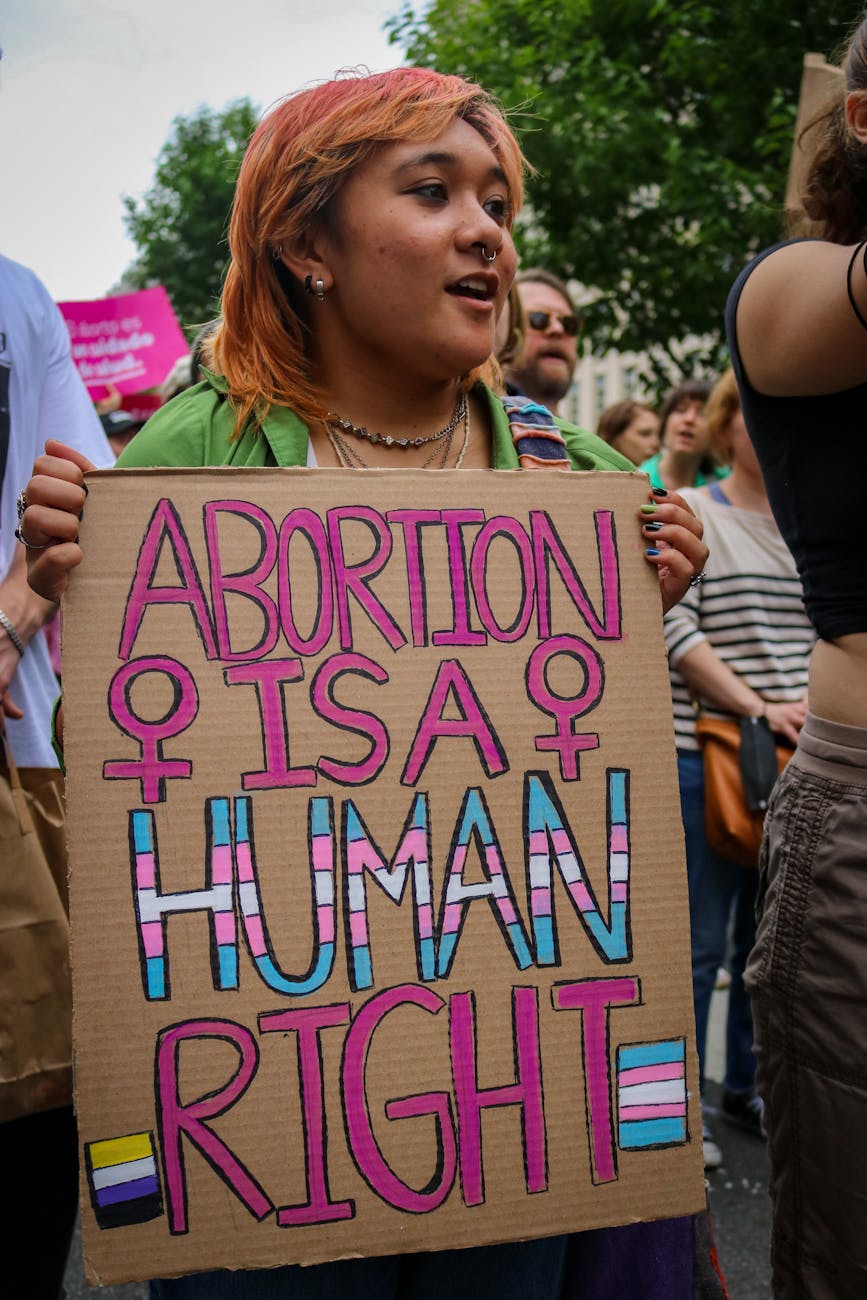
Reproductive health is more than just abortion – it’s also preventative primary care, birth control, cancer screenings, fertility treatments, and safe access to abortion procedures. The right to one’s body, or autonomy, is tied to reproductive healthcare and gender-affirming services. Despite the shame and hate tied to these fields, few services are linked to human rights and equality worldwide.
Looking for general information about non-reproductive medical healthcare or health insurance? Click here.
WHAT EXACTLY IS BODILY AUTONOMY?
Bodily autonomy refers to one’s right to make decisions about their own body, life, and future without violence, coercion, or persecution. It’s thrown around frequently when discussing reproductive health and gender-affirming care, but it’s a fundamental human right that is foundational to gender equality. Without bodily autonomy, individuals can’t choose whether they want to be married, have sex, use condoms, go to the doctor, or be pregnant.
Bodily autonomy is tied to certain laws around the world, like age, ability, or gender. In the United States, children are denied bodily autonomy for most medical decisions until they turn 18 – they’re only able to see a medical provider under their parent’s supervision and decision rather than their own. Likewise, disabled people of any age are generally denied bodily autonomy – so it’s not uncommon for disabled people to be denied the ability to marry or have sex because other people like their parents or guardians get to make that decision for them. In countries like South Sudan, women are denied the bodily autonomy to deny or reject marriage (or get divorced) since their families make those decisions on their behalf. Likewise, in places like Egypt, transgender people are denied the bodily autonomy to gender-affirming care such as hormone replacement therapy.
Author’s Note: All aspects of reproductive health and gender-affirming care are rather unstable due to the national political stage. It’s unlikely (but not impossible) for a nationwide ban on care, but it is likely for national protections to be removed – making it difficult to find abortion or gender-affirming care in hostile states.
Birth Control & Contraception
Contraception is the technical term for “birth control,” which is any medication, device, or surgery that prevents pregnancy. Birth control techniques can be temporary, reversible, or permanent – and a few also prevent sexually transmitted diseases (STDs). They achieve this by killing sperm, making a physical barrier between the sperm and egg, preventing eggs from being released in the ovaries, and altering the uterus tissue so fertilized eggs can’t be implanted.
Types of Birth Control
Intrauterine devices (commonly referred to as IUDs and IUCs) are one of the most effective kinds of birth control available. There are five main brands approved by the FDA for use in the United States: Paragard, Mirena, Kyleena, Liletta, and Skyla – most of which are hormonal-based and use the hormone progestin to prevent pregnancy, whereas Pargard is wrapped in copper to prevent pregnancy instead of hormones. As a result, Paragard IUDs prevent pregnancy up to 12 years while hormone-based ones range from 3 to 8 years.
- The reason Paragard works so well is because sperm naturally dislike copper, so it’s a natural non-hormonal deterrent that creates an internal barrier between the egg and sperm.
- Since copper-based IUDs don’t use hormones associated with other birth control methods, it’s often a common choice among transmasculine people since it won’t interfere with hormone replacement therapy or their gender-affirming care.
- Progestin mimics the progesterone that bodies naturally make, which will either thicken the cervix mucus to physically block and trap sperm or prevent ovulation entirely.
IUDs are highly recommended for pregnancy prevention since they’re extremely low-maintenance, highly effective, long-lasting, and reversible. After being inserted by a medical provider, you’re covered by a 99% effectiveness rate until it’s removed – there are no daily pills to take, days to track, or mistakes to avoid.
Birth control implants, or Nexplanon, are another highly effective and low-maintenance form of birth control that prevents pregnancy up to five years after it’s originally inserted. Just like IUDs, implants release the hormone progestin to prevent pregnancy – but instead of being inserted in the cervix, the implant is placed in the upper arm. Compared to IUDs, implants aren’t associated with as much pain during insertion since numbing agents are used to ease the process – but implants aren’t covered by as many government programs to be offered for free as IUDs.
Birth control or depo shots are injections received once every three months – but unlike IUDs and implants, depo shots can occasionally be done at home without a doctor’s appointment. Just like most IUDs and implants, birth control shots use progestin to prevent pregnancy. While shorter lasting, the shot doesn’t require anything to be implanted or inserted but it must be taken every 12 to 13 weeks to remain effective. Additionally, birth control shots are massively easier to pay for out-of-pocket without insurance or government programs – the IUD can cost up to $1,800, the implant can range upwards of $2,300, but the shot costs $150 at most.
Did you know birth control can also be taken as a vaginal ring? The birth control ring is a small, flexible ring placed inside the vagina to prevent pregnancy for up to a month at a time – which has some caveats. As such, the ring and other forms of birth control have lower effectiveness rates than IUDs and implants since they require more upkeep and are accident-prone. That being said, the ring is still 93% effective when used correctly. There are two main types of birth control rings:
- NuvaRing is capable of stopping periods and is replaced every month. It lasts up to five weeks at most, so if you forget to replace it, you’re at risk of becoming pregnant.
- Annovera rings are used for three weeks before being removed for seven days. After one ring-free week, the Annovera ring is re-inserted into the vagina. While NuvaRings have to be discarded each month, Annovera rings last one year each if used on schedule – but they don’t stop periods.
Both ring types prevent pregnancy by stopping ovulation through the use of estrogen and progestin, which is absorbed from the ring into the vaginal lining. Like IUDs, implants, and the shot, a prescription is required – but unlike them, you have the freedom (and responsibility) to take the ring on your own time.
The birth control patch is another safe and convenient option, where a prescribed transdermal patch is worn on the skin to prevent pregnancy by releasing estrogen and progestin just like traditional birth control pills. The patch must be replaced weekly to be effective and only work if they’re stuck properly – so no lotion, creams, powders, or makeup can be used near them and you can’t be sensitive or allergic to its adhesive. All forms of birth control that are taken on your own, such as the ring, patch, or pill, can be prescribed online by telehealth.
The most popular form of birth control today is the pill, a 93% effective oral medicine that prevents pregnancy if taken every day. Once approved by the FDA in 1957, the pill had a profound effect on feminism and women’s sexual liberation since it was the first mainstream medicine that allowed them to choose motherhood. Birth control is covered by nearly all American health insurance and welfare plans, and Opill has been the national form of birth control available over-the-counter without a prescription or doctor’s visit since 2024.
Those aren’t the only options for birth control, either – some additional (but less common) forms include:
- Cervical caps are soft silicone cups placed deep inside the vagina to cover the cervix, creating a physical barrier between sperm and the egg. A prescription is required and they’re around 71% to 86% effective – but they work even better when used with spermicide. Smaller than the diaphragm, cervical caps can be left for up to two days before being removed.
- Diaphragms are soft silicone cups that are bent and then inserted into the vagina to cover the cervix, creating a physical barrier to stop pregnancy. Like cervical caps, a prescription is required for diaphragms. They can’t be left inside the vagina as long as caps, but they’re generally more effective (83%) since they don’t have the larger range caps do. Similar to cervical caps, diaphragms work best when used with spermicide.
- Contraceptive sponges are made from soft, squishy plastic that’s placed inside the vagina before sex to cover the cervix, creating a barrier to prevent sperm from reaching the egg and causing pregnancy. Sponges vary from 78% to 86% effective and need spermicide to work best – but unlike cervical caps and diaphragms, contraceptive sponges don’t require a prescription.
- Spermicide and contraceptive gels contain chemicals that stop sperm from reaching the egg, placed inside the vagina before sex. It ranges from 79% to 86% effective at preventing pregnancy and doesn’t require a prescription – it’s found over-the-counter at most drugstores, pharmacies, and supermarkets. However, spermicides don’t work on their own; you have to use a diaphragm or cervical cap alongside it.

Condoms are thin pouches that create a physical barrier between genitals during sex, and they’re the only option that prevents both pregnancy and sexually transmitted diseases. External or male condoms are worn on the penis, collecting semen and preventing sperm from reaching the egg. Internal or female condoms are worn inside the vagina or anus, similarly collecting semen. Condoms must be worn every time you have sex to be effective. Remember you should always check condoms’ expiration date before use, look for potential tears, and never store condoms in hot or cold places or direct sunlight – and double-layering condoms increase the risk of a tear or breakage, not protection.
- Most condoms are made of latex rubber, which can be found in any supermarket, pharmacy, online, or at health centers. They’re also the cheapest, so they’re offered for free at many organizations. Latex condoms can only be used with water and silicone-based lube – oil-based lubricants can damage latex condoms. Note that silicone-based lube can damage silicone toys and prosthetics, so check your items prior to use.
- Plastic latex-free condoms are made from materials like polyurethane, nitrile, and polyisoprene to create an alternative that’s better suited for individuals with latex allergies. However, plastic condoms are slightly more expensive than their latex counterparts so they’re not as commonly found in some regions. Water and silicone-based lube is best suited for plastic condoms, although oil-based lube can be used for any plastic condom not made from polyisoprene.
- Internal condoms are made from plastic, not latex – so the same rules apply. Latex and animal skin condoms are not options for female condoms.
- Lambskin and animal skin condoms are made from the lining of the intestines, but they’re only able to prevent pregnancy. Compared to other condom alternatives, animal skin condoms don’t prevent STDs due to the materials used. Unlike other condoms, lambskin condoms can be used safely with any type of lube.

Experts advise regular use of both condoms and birth control for sexually active individuals at risk of pregnancy. In relationships where pregnancy isn’t possible, condoms and/or PrEP should still be used since STDs don’t discriminate against gender identity or sexual orientation.
In religious areas, abstinence is recommended as the most (and only) effective form of birth control. While abstinence (or the act of not having sex) and outercourse (sex that doesn’t involve penis-in-vagina penetration) are the only methods that are 100% effective at preventing possible pregnancies, they’re not the best number one form of birth control since most people will have sex at some point in their lives.
- Outercourse can prevent pregnancy, but it can’t prevent STDs. Remember to wear a condom if STDs are a potential risk.
- Some people purposely don’t have sex or become temporarily abstinent when they’re at risk of becoming pregnant based on their menstrual cycle. This is called “natural family planning,” “the rhythm method,” and fertility awareness methods (FAMs) and requires a higher level of dedication since it’s your personal responsibility to track ovulation.
In a similar vein, some individuals practice the withdrawal method as their primary form of birth control – also referred to as pulling out. By pulling out the penis from the vagina before ejaculation (or cumming), pregnancy can be prevented since sperm is physically kept from the egg. Pulling out only works when done correctly before ejaculation since any amount of semen (no matter how little) can cause pregnancy if inside the vagina. It doesn’t prevent STDs, and it’s notoriously difficult to do correctly – leading it to have lower efficacy rates than other birth control methods.
One large reason condoms and birth control practices like those mentioned above are considered best is because pregnancy and STDs can also occur from precum – meaning before ejaculation. While the chances are low, it is possible to become pregnant from precum since sperm mixes with the alkaline fluid in the urethra. In other words, pregnancy can still happen even when you perform the withdrawal method perfectly since just one viable or healthy sperm is needed to fertilize an egg.
The last non-permanent form of birth control is breastfeeding since regular breastfeeding stops the body from ovulating and therefore prevents pregnancy. It’s also called the lactational amenorrhea method (LAM) because it also naturally stops the period and works at similar rates as oral birth control pills. However, LAM only works if you’re breastfeeding – which requires you to have recently been pregnant.
There are two main types of permanent birth control, referred to as sterilization. They are 99% effective at preventing pregnancy (but not STDs). These are not reversible and considered life-long decisions – which is why they can be difficult to access since the economy and government have a weighted interest in forcing young people to have children. On the other hand, certain groups of individuals have been targeted for forced or coerced sterilization like women of color, disabled people, and transgender people.
- Individuals assigned female at birth can undergo tubal sterilization (“getting the tubes tied”). There are three subtypes of tubal ligation, which all physically prevent sperm from reaching a viable egg by blocking or removing the fallopian tubes.
- Tubal ligation surgically closes, cuts, or removes pieces of the fallopian tube.
- Bilateral salpingectomy removes the fallopian tubes entirely.
- Essure sterilization uses a tiny coil to block the fallopian tube – while it used to be a common form of sterilization, essure sterilization is no longer available in the United States.
- Individuals assigned male at birth can opt for a vasectomy, a procedure where the small tubes inside the scrotum are cut or blocked that carry sperm.
- Incision vasectomy utilizes one or two small cuts on the vas deferens by tying, blocking, cutting, or closing with electrical currents. It is an extremely fast procedure that takes about 20 minutes before it’s stitched up.
- No-scalpel vasectomy requires the doctor to make one small puncture to both of the vas deferens tubes before tying off, blocking, or cauterizing the tubes. Since the skin isn’t cut with a scalpel, there’s no need for stitches or scarring and it heals quickly.
Accidents Happen: Emergency Contraception
Birth control prevents pregnancy ahead of sex, relying on the various methods above to be used before/during sex. In contrast, emergency contraception prevents pregnancy after sex- most EC is 95% effective up to five days after unprotected sex (as well as other reasons for emergency contraception like contraception failure, incorrect use of birth control, or assault).
Emergency contraceptive works by temporarily stopping the body from releasing an egg, preventing ovulation that puts you at an increased risk of pregnancy. Pregnancy doesn’t happen immediately after sex nor does it happen every time you have sex – that’s why EC works and why it is different from abortions.
IUDs are more than just birth control: they’re considered one of the most effective forms of EC. Unlike other emergency contraceptives, IUDs don’t decrease in efficiency if taken within five days – they’re just as effective at preventing pregnancy on day five as they are on day one. And as an add-on, IUDs aren’t weight-based and work for all body sizes. On the downside, it’s more difficult to get an appointment for an emergency IUD compared to the following EC pills.
There are two types of “morning-after pills,” which are the more commercially available forms of emergency contraception available for purchase. It is important to note that emergency contraceptive pills work best when taken as soon as possible after sex because their effectiveness decreases with time, even if you’re within the appropriate five-day span.
- Ulipristal acetate-based pills (brand name Ella) are the most effective EC pills but require a prescription. It can be taken up to 120 hours after sex and works best for individuals who weigh 195 pounds or less.
- All forms of morning-after pills don’t work if you’re already ovulating. Ella is capable of working closer to ovulation, but an IUD may be a better EC option if you’re ovulating.
- Levonorgestrel-based pills (brand names Plan B, Take Action, My Way, Option 2, AfterPill, etc.) are available over the counter at any drugstore, pharmacy, or supermarket. It should be taken within 72 hours after sex – it works best for individuals 165 pounds or less, although it’s not uncommon for people who weigh more to take an additional dose.
- There’s a lot of misinformation about Plan B and its variants (often on purpose to confuse buyers and those in need). Since 2013, there hasn’t been an age requirement to buy Plan B over-the-counter – regardless of where you are in the United States. Some stores may lock Plan B in security packaging to deter theft, but it can be purchased any time of the day and can’t be restricted if the store is open. No IDs are necessary to buy Plan B, either.
- Under the Affordable Care Act, most commercial insurance plans fully cover Plan B as well as government alternatives like Medicaid. However, having insurance or Medicaid pay for Plan B requires a prescription.
- Out of pocket, Plan B costs about $40 over the counter. Pro-tip: it’s significantly cheaper to buy Plan B ahead of a crisis, like via Amazon, but it will take longer to arrive while it ships. Part of the reason Plan B can sell so high is due to demand since $40 is still significantly less than the cost of having a baby. There’s also select organizations and programs that provide Plan B for free (listed below in Additional Resources), although their supply is limited.
In an emergency and other options are unavailable, regular birth control pills can work as emergency contraceptives and prevent pregnancy after sex since they use the same hormones in lower doses. You’ll want to make sure you take it in two rounds, and the number of oral birth control pills needed will vary based on its formula.
Emergency contraceptive pills are considered extremely safe. They’ve been around for over 30 years and haven’t had any reports of serious complications. EC doesn’t have any long-term side effects and won’t have any impact on your ability to potentially get pregnant in the future.
It is not advised to use two different kinds of morning-after pills at the same time, such as Ella and Plan B. By doing so, they may counteract and not work at all.
Emergency contraceptives shouldn’t be used in replacement of regular birth control methods. While it’s safe to take EC pills multiple times as needed, it’s not as effective at preventing pregnancy – it’s also significantly more expensive.
Unsure about what emergency contraceptive method is best for you? Planned Parenthood has a short quiz that uses details about your age, weight, and last time you had sex to recommend the best options available.
Reproductive Healthcare is Healthcare
Health is a state of complete physical, mental, and social well-being – which includes reproductive wellness. Nearly all of the clinics and organizations that provide abortion services and birth control also offer in-depth services for reproductive health, which is why entities like Planned Parenthood are important.
Reproductive healthcare refers to the services provided to support one’s physical, mental, and social well-being concerning one’s reproductive system. Most diseases are preventable or treatable if caught early, so seeing a healthcare provider regularly is critical to staying healthy. Everyone should see a provider annually for screenings best suited for their age and health – and all sexually active people should be tested every three to twelve months depending on their risk factors.
- Sexually transmitted infections (STIs) and diseases (STDs) spread during vaginal, anal, oral, and blood-to-blood contact. All STDs are treatable, and most are completely curable – but only if you get care from a healthcare professional. Most STDs do not have any symptoms, which is why regular testing is a necessary commitment for sexually active people to stay healthy. Otherwise, you are at risk of serious health problems later in life! They can be tested through blood samples, urine tests, saliva swabs, spinal tabs, and visual examinations. It varies by jurisdiction, but most US states allow people ages 13 and older to be tested and treated for STDs without parental consent.
- Vaccines exist to prevent STDs like hepatitis B and HPV, which are given to most children in the United States around age 11 or 12. These vaccinations are recommended for all young people regardless of gender since these illnesses do not discriminate based on gender.
- Regular self-exams are necessary in order to know what your “normal” is – everybody is unique and covered in various lumps and bumps, so self-examining your body lets you know when something is potentially wrong and worth professional attention.
- People of all genders should know what their breast tissue normally feels like through breast self-exams (BSEs). Everyone, including cisgender men, has breast tissue – which is capable of producing cancer. Individuals with a high family risk of breast cancer as well as all women 40 or older are recommended to get mammograms, which can detect cancer in its earliest stages when it’s most curable.
- Folks with uteruses need to get pelvic or internal exams once they turn 21 years old, which requires a doctor’s visit where a professional examines the vulva, vagina, cervix, ovaries, fallopian tube, and uterus. Pelvic exams are recommended annually, whereas pap smears (which are different from pelvic exams) are advised every three years to check for early signs of cervical cancer.
- Individuals with testicles need to do a testicular self-exam (TSE) at least once a month at age 15. That’s much younger than most people realize or what most public schools teach, but AMAB individuals are at the greatest risk of testicular cancer from the ages of 15 to 35.
- People with prostates get prostate or rectal exams when there’s an issue with the anus, prostate itself, or constipation. Younger folks only get prostate exams if there’s a cause or concern, but anyone with a high risk of prostate cancer or age 55 or older is recommended to get a prostate exam annually.
Infertility is characterized as the inability to cause a pregnancy despite regular unprotected sex. The World Health Organization estimates that 17.5% of adults experience infertility issues, which translates into 1 in 6 adults. Healthcare providers can perform semen analysis, hormone testing, genetic testing, thyroid testing, biopsy, imaging, hysterosalpingography, and other methods to determine if someone is experiencing infertility.
As an aside, hormone replacement therapy can have long-lasting and permanent effects on fertility among transgender people. While puberty blockers do not affect fertility, the use of HRT can make someone incapable of having biological children later in life – which is why aspiring trans parents can freeze sperm and eggs for later use. Temporarily pausing HRT can improve fertility, although it is generally believed that the longer someone is on HRT, the more likely they will become infertile regardless.
Infertility for individuals assigned male at birth revolves around a lack of healthy sperm. As a result, men are prescribed lifestyle changes as a first step to resolving infertility – although lifestyle and habits play a significant role in anyone’s fertility regardless of gender. Some of these prescribed habits include more frequent sex, increased exercise, diet changes, and stopping alcohol and nicotine use alongside other substances. While many of these are manageable, some lifestyle impacts are difficult to control – like one’s exposure to radiation or pesticides in their environment or neighborhood, which is known to cause infertility.
- Half of male infertility cases have no determined cause – it’s a complex issue that can be influenced by countless factors like genes, hormones, and lifestyle.
- Age 40 is the general guideline when cisgender men are expected to become naturally less fertile. The decrease in fertility is relatively insignificant at 40, although it gradually increases with age.
- Unresolved sexually transmitted diseases account for a chunk of male infertility problems since STDs like chlamydia and gonorrhea are notorious for doing so. Individuals assigned male at birth are less likely to experience symptoms associated with STDs like chlamydia, but regular testing is important since later infertility issues can still occur if the infection is not treated.
- Physical blockages can naturally occur similarly to how vasectomies purposely prevent pregnancy. In these cases, surgery can be performed to reverse the blockage and restore fertility.
- Some medications cause infertility, although you should only stop taking a prescribed medication under the direction of your healthcare provider after discussing fertility options. There are also several medicines available to promote male fertility, which often boost testosterone levels and lower estrogen levels as a means to promote sperm production. However, synthetic testosterone (medication that is prescribed to transmasculine people as HRT or to cisgender men experiencing conditions like erectile dysfunction) does not help with male infertility – the medical consensus is that synthetic testosterone lowers male fertility rates.
- Lastly, a doctor may recommend assisted reproductive techniques like IUI or artificial insemination – individuals produce a semen specimen to be processed, drastically increasing the concentration of healthy sperm before it’s placed into a uterus before ovulation. While IVF is more popular with lesbian same-sex couples (as described below), other assisted reproductive techniques include cryopreservation and surrogacy – which is employed by many gay same-sex couples otherwise unable to have biological children.
Individuals assigned female at birth can also experience infertility issues. The same lifestyle changes suggested for men can also promote female fertility, such as bettering nutrition and quitting cigarettes.
- Between 20% to 30% of female infertility causes have no established cause, although this estimate fluctuates by source.
- There’s more misinformation regarding female infertility and age, especially since there is an economic interest in having women pay for fertility treatments. 35 is the estimated age when female fertility begins to decline – but it’s a gradual continuum like men’s fertility. Language like “geriatric pregnancy” purposely tries to scare women into having children young, even if they’re unsure about parenthood. The limited research out there actually proposes the decline is nowhere as extreme as the fertility industry wants you to believe – one of the largest studies on the subject found 73% of women between the ages of 34-40 naturally conceiving within one year of regular sex at least twice a week. That’s not much lower than the 88% of women aged 30-34 or the 84% of women between 25-29. Female fertility is complex!
- Pelvic inflammatory disease (PID) is a complication associated with untreated STDs that damage and scar the fallopian tubes, leading to infertility since it obstructs the egg from traveling to the womb for fertilization.
- Hormone and ovulation issues are the most associated with female infertility since conditions like polycystic ovary syndrome (PCOS) and thyroid-related diseases prevent ovulation. Both an overactive and underactive thyroid gland prevents ovulation.
- While ovulating, the cervix naturally produces thinner mucus to allow sperm to swim more easily. Some female fertility issues stem from problems with the cervical mucus itself since it can make it harder to conceive.
- Non-cancerous growths called fibroids can affect fertility, especially when they’re in or around the womb since they can block the fallopian tube or prevent a fertilized egg from attaching to the womb. Endometriosis is also associated with female infertility, where tissue similar to the endometrium lining of the womb grows in places other than the womb – eventually damaging the ovaries and fallopian tubes. Hysteroscopy and related surgeries can improve fertility by removing scar tissue, polyps, and fibroids, while laparoscopic surgery can treat large fibroids and infertility caused by endometriosis.
- Certain medications have negative impacts on fertility, like non-steroidal anti-inflammatory drugs (NSAIDs), neuroleptic drugs, and other substances. There are several medications used to promote female fertility, like clomiphene citrate, gonadotropins, metformin, letrozole, and bromocriptine.
- The assisted reproductive technique recommended for women is in vitro fertilization (IVF), although this procedure is ongoingly under attack by religious conservatives in America. During IVF, eggs are taken from the ovaries to be fertilized by sperm in a lab – after they’ve developed into embryos, they’re placed into the uterus to resume pregnancy. IVF is especially popular with same-sex couples alongside surrogacy and egg/embryo donation.
Reproductive healthcare also includes prenatal care, which refers to the specialized services given during pregnancy to promote both the health of the pregnant person and the baby. Without prenatal care, it’s impossible to know the pregnancy is staying on track and ensure the baby is healthy, which is why ultrasounds and testing are used to gauge health. Tests like amniocentesis check for certain birth defects, while chorionic villus sampling tests for genetic abnormalities that can happen during pregnancy.
It takes more than just one doctor to ensure a healthy pregnancy – doulas are non-medical professionals trained to guide a pregnant person and their family. The use of a companion during childbirth dates back to prehistoric times, and doulas provide support with childbirth, miscarriages, induced abortions, stillbirth, and death. Similarly, midwives are medical professionals who can provide care and medicine to pregnant people, new mothers, and newborns. Midwives are used for ultrasounds and are best for monitoring the progress of labor – the defining difference between midwives and doulas is that doulas provide more emotional support but are unable to practice medicine like certified midwives.

Abortions are Healthcare
One-quarter of women will have an abortion by age 45 for a variety of reasons – like already having children, health issues, money, being in school, not wanting kids, etc. There’s no singular reason, and they’re all valid reasons to not want to pursue parenthood. Abortions are medical procedures that terminate a pregnancy.
- Mifepristone and misoprostol pills are effective at terminating pregnancies that are at ten weeks or fewer, forcing the body to expel the pregnancy tissue in the uterus. The pills are known for feeling unpleasant, causing intense cramping and bleeding for several hours related to the length of the pregnancy. Pill abortions range from 94% to 98% effective at terminating pregnancy, but require a health center’s approval for the prescription. The effectiveness of the pill decreases the further along a pregnancy is unless an extra dosage is prescribed. Unlike emergency contraception, there are no over-the-counter options for abortion.
- Suction abortion or vacuum aspiration is the most common in-clinic abortion procedure with a 99% effectiveness rate. It’s performed on pregnancies between 14 to 16 weeks along and gently sucks the embryo/fetus from the body.
- Pregnancies at 16 weeks or more must be terminated by dilation and evacuation, which uses a combination of suction and medical tools to remove the fetus. It also maintains a 99% efficiency rate like vacuum aspiration.
All-Options is a toll-free talkline that can be reached at 888-493-0092, giving professional emotional support and resources on pregnancy, adoption, parenting, infertility, and abortion in a non-judgemental space and more advisable than traditional “abortion hotlines,” which use misinformation to scare callers.
Most abortions occur in an abortion clinic or hospital, although they can be performed in a variety of settings. Planned Parenthood is most known for abortion services, but they’re also the leading provider of all reproductive healthcare services in the United States. AbortionFinder is the best way to find a provider near you, which uses information based on your location, age, and pregnancy state to recommend nearby legitimate clinics. When seeking information about abortion, it’s important to look out for crisis pregnancy centers (CPCs) or “fake clinics.” CPCs and mobile vans look exactly like real health centers but are run by anti-abortion activists to promote their agenda and scare, shame, and pressure individuals into continuing their pregnancies. After promising to provide pregnancy testing, counseling, and STD testing, they use false information to miseducate people about abortions, birth control, and sexual health – and they do everything in their power to look legitimate by using biased doctors, providers, and researchers (who have been kicked out of the larger legitimate scientific community). Since CPCs are not real clinics, they are not required to adhere to any of the laws real clinics have to – like HIPAA. It’s not uncommon for CPCs to share personal and private information with other organizations and CPCs to continuously harass you. The Anti-Abortion Pregnancy Center Database, Crisis Pregnancy Center Map, and Expose Fake Clinics all have maps with location-based data on CPCs – although CPCs often change their names and locations frequently to confuse the public.
63% of all US abortions are done by mifepristone and misoprostol pills, meaning 6 out of 10 abortions occur within the first 10 weeks. After 10 weeks, the baby is considered a fetus with all of its major organs formed and beginning to function. 93% of all abortions happen in the first trimester (within the first 13 weeks of pregnancy), while the CDC found in 2019 that less than 1% of abortions occur during the third trimester (28 weeks and more).
These numbers indicate that despite the false rhetoric by anti-abortion activists, third-trimester abortions are extremely rare. Most often, these late-term abortions happen because of health concerns or other causes unrelated to simply “not wanting” a pregnancy. By the third trimester, the majority of pregnant individuals have already had their baby shower, have told their friends and family members of their upcoming birth, and very likely have names picked out. All abortions are necessary since first-trimester abortions prevent unwanted pregnancies that are at a higher risk of poverty, illness, and abuse in homes unable to sustain them whereas third-trimester abortions are medically necessary to preserve the life of the would-be mother.
The overturn of Roe v. Wade means that each state is given the complete freedom to determine which abortions are legally allowed to be performed – if any. Before the Supreme Court’s decision, every state had to legally permit abortion in some capacity although they were still given the freedom to regulate abortion past the first trimester. This has led to some horrific situations that the rest of the world looks down upon – like forced pregnancies by children through rape and incest. There are states with no minimum protections, and political figures that claim to be protecting children from LGBTQIA+ people actively cause them harm – such as the 10-year-old who made national headlines when she had to travel from Ohio to Indiana for an abortion after being raped post-Roe.
There’s a lot of political discourse that could be written here, but the short version is that religious and conservative groups are disproportionally more likely to assault, groom, and generally harm children through abuse, rape, and legislation than queer and transgender people. However, a growing number of conservative-controlled states are entirely banning abortion in all forms and criminalizing the act – as well as calling for a national abortion ban to criminalize abortion outside of their own state jurisdiction. The Center for Reproductive Rights has a live map with information on abortion laws and protections throughout the United States, detailing its legality in all states and territories.
Additional Resources
2 + Abortions is a collection of stories, support groups, and testimonies of individuals who have had two or more abortions in their lifetimes. Their website is geared to dismantled the stigma and shame associated with abortions.;
Abortion Care Network is a national association of independent community-based abortion care providers, which make up the majority of abortion professionals in the United States.
Abortion Diary Podcast is a story-telling platform to share the experiences of the millions of people who have had abortions.
Abortion Finder is a search tool to connect users with over 750 verified abortion providers across the United States, using information like age, location, and last menstrual cycle to list clinics.
Abortion Out Loud is a national network through Advocate for Youth to support young people in need of abortion services or support.
Abortion on Demand provides abortion pills via mail around the US in judications where they are legally allowed to do so through telehealth.
Abortion on Our Own Terms is an advocacy campaign that seeks to change the culture surrounding abortion – especially self-managed abortion done through abortion pills.
Abortion Resolution Workbook is a free resource for individuals wanting self-help with emotional and spiritual conflict after an abortion.
ACLU Reproductive Freedom Project is a litigation and advocacy program of the American Civil Liberties Union to uphold the rights of individuals to freely seek sexual education, contraception, abortion, prenatal care, and childbearing assistance.
Advancing New Standards in Reproductive Health is a research program based at the University of California San Francisco that conducts multidisciplinary research on sexual and reproductive health.
Advocates for Youth is a collective for youth people’s access to reproductive and sexual health, which partners with thousands of youth-focused organizations around the country.
Aid Access facilitates online abortions in all US states with FDA approved abortion pills. The site uses telehealth alongside licensed providers to mail abortion pills to be used at home.
Alliance for Period Supplies hosts a network directory of organizations throughout the United States that provide free period products like pads and tampons.
All-Options, formerly known as Backline, is a toll-free talkline for abortion, pregnancy, parenting, and adoption support available in the United States and Canada.
AMAZE is a free series of sexual health videos hosted on YouTube that uses animation to education young people, parents, and teachers with age-appropriate content.
American College of Obstetricians and Gynecologists is a professional association of providers that are specialized in obstetrics and gynecology to ensure best medically accurate and up-to-date practices in the field.
American Sexual Health Association operates Yes Means Test, a free tool that allows users to find free and confidential STD testing throughout the country based on their zip code and CDC information.
Apiary for Practical Support is an online directory of organizations across the US that provide logistical assistance for people seeking abortion, referred to as Practical Support Organizations (PSOs).
Bedsider is an online birth control support network for individuals between the ages of 18 to 29 through Power to Decide, which explains various birth control methods with comprehensive information.;
Centers for Disease Control and Prevention (CDC) is the official national public health agency of the United States that operates under the Department of Health and Human Services to control, prevent, and treat disease, injuries, and disability in the general public. The CDC is staffed by the current presidential administration to tackle ongoing health concerns and educate the American public.
Center for Excellence in Transgender Health advances health equity and research among transgender and nonbinary communities through the University of California San Francisco.
Center for Reproductive Rights is a global human rights organization that uses partnered attorneys and advocates to ensure reproductive rights are protected in law. Their websites maintains comprehensive information about reproductive health and abortion laws to help users visualize data.
Condom Collective is an Advocates for Youth program made up of youth-led grassroots movements to normalize condom use on college campuses by distributing free condoms and sexual health information.
Doctors Without Borders is an international non-governmental organization that provides free medical and mental health care to people in need, including abortion services in crisis communities they serve.
Ending a Wanted Pregnancy is a group for individuals who made the decision to end a wanted pregnancy, often due to a poor prenatal diagnosis or maternal health reasons.;
Exhale Pro-Voice is a confidential textline available in the United States and Canada for post-abortion emotional support. While Exhale Pro-Voice does not sell abortion pills, they provide professional counseling support.
Fòs Feminista is an alliance of over 250 organizations around the globe that work to advance sexual and reproductive health, rights, and justice.
Guttmacher Institute is a leading research and policy organization that provides data on reproductive topics like abortions, contraception, and STDs.
How to Use Abortion Pill is an online community that shares facts and resources on the abortion pill, such as how to access and use the pill and what to to expect while having a pill-based abortion.
If/When/How is an association and movement for lawyers dedicated for reproductive justice, which also provides funding for bail and legal fees associated abortion, pregnancy issues, immigration, and criminal law.
I Need An A uses non-personally-identifiable information to connect users temporarily with abortion providers most relevant for their circumstance, which is deleted and not stored afterwards. I Need An A works with organizations like Abortion Care Network, Apiary for Practical Support, and the National Network of Abortion Funds to be a starting point for individuals unsure where to begin regarding abortion care.
Ipas is an international non-governmental organization that improves access to abortion and contraception around the world, especially in Africa, Asia, and Latin America.
Ipis Reproductive Health conducts research to advance sexual and reproductive health rights around the world, such as in the United States, Latin America, Caribbean, and Africa.
Just the Pill is a mobile telehealth clinic that mails abortion pills, contraception, and other sexual health services to users in select US states.;=
Love is Respect is a project of the National Domestic Violence Hotline that serves as the national resource in the United States regarding domestic violence for young people ages 26 and younger.
Marie Stopes International, also known as MSI Reproductive Choices, works in 36 countries to provide reproductive healthcare such as birth control and abortion.
Miscarriage + Abortion Hotline is a free hotline for people seeking information and support on abortion and miscarriages through experienced healthcare professionals.
Out2Enroll connects LGBTQIA+ people and their families with any and all healthcare coverage options through the Affordable Care Act, including Medicaid, Medicare, and commercial insurance. O2E helps users compare plans based on LGBTQIA+ factors, like gender-affirming care or coverage for same-sex partners.
Our Bodies Ourselves is a comprehensive website that provides information on sexual health topics, including abortion, birth control, menstrual cycles, menopause, pregnancy, and more. The site also writes related news articles and posts about topical sexual health information and events.
National Abortion Federation is a professional association of abortion providers, which includes private and public providers. NAF also hosts the National Abortion Hotline – the largest toll-free multi-lingual hotline for abortion information in the US and Canada.
National Family Planning and Reproductive Health Association is a membership organization for providers and administrators committed to helping people find family planning information.
National Network of Abortion Funds is a directory of organizations that provide financial assistance for individuals seeking abortion care. There is a large number of financial providers across the United States, but they operate in small localized regions – so NNAF connects users to relevant organizations they are eligible for.
Pills by Post is a trusted online abortion pill provider that uses telehealth to prescribe abortion services in select approved states. While they operate in less state than other online abortion providers, Pills by Post is significantly cheaper if paying for services out of pocket.
Plan C Pills connects users with online abortion providers in all US states, although they do not directly provide abortion pills themselves. Plan C Pills provides abortion advice and options for all users, even in states where abortion is completely banned and criminalized.
Planned Parenthood is the largest reproductive health services provider in the United States. Although not an FQHC, Planned Parenthood has several safety nets in place to see patients regardless of their ability to pay. In addition to screenings, gender-affirming care, and abortion services, Planned Parenthood also provides free condoms, emergency contraception, and sexual education – including trained counselors available via online chat.
Power to Decide operates a number of other important resources included in this list, like AbortionFinder and Bedsider, as well as other initiatives aimed to advance reproductive health in the United States.
Reddit is a social media platform that operates through thousands of forums (referred to as subreddits) for users to find related communities and discussions. Relevant subreddits include: r/abortion, r/STD, r/auntienetwork, r/antinatalism2, r/prochoice, r/pregnant, r/Miscarriage, r/birthcontrol.
ReproCare is an anonymous healthline that provides accurate information and emotional support about reproductive and sexual health.
Reproductive Freedom for All mobilizes activists and allies to fight for better access to abortion, birth control, paid parental leave, and protections from pregnancy discrimination.;
Reproductive Health Access Project trains and supports healthcare providers to create health equity within the sexual wellness and reproductive healthcare field.
Repro Legal Helpline provides free legal advice about abortion, pregnancy loss, and birth. In addition to their telephone services, their website also provides guidance on abortion laws and policies, as well as associated protections and criminalization.
Resources for Abortion Delivery gives grant funding, technical assistance, and legal compliance assistance to abortion providers in the United States.;
Safe2Choose is an online community that supports individuals seeking abortion with counseling and information with pro-choice healthcare providers.
Safe Abortion Access Fund is a global fund that provides financial support to low and middle income countries around the world in need of abortion advocacy, research, and attitude-transformation.
Scarleteen is a massive online resource and advice website for comprehensive LGBTQIA+-inclusive sexual and relationship education. They have been operating their message boards, advice columns, live chat, and text service for decades.;
Self-Managed Abortion Safe and Supported is a project of Women Help Women to support the rights of people seeking information and access to abortion in the United States.
Sex, Etc. improves teen sexual health through free education resources, videos (like AMAZE), glossaries, and advice to connect young people with accurate data on sex, relationships, pregnancy, STDs, birth control, sexuality, gender identity, etc. It’s operated by Answer, a national organization that promotes sexual education for all ages.
Sexuality Information and Education Council of the United States, or SIECUS, is an advocacy, policy, and coalition building organization that works to advance American sex education.
SisterSong Women of Color Reproductive Justice Collective is a national membership organization for individuals and organizations centered on improving reproductive policies that impact marginalized communities – such as women of color.
United States Department of Health and Human Services Office of Population Affairs is the official government US government agency that handles family planning and population services.
United Nations Population Fund is the official agency under the United Nations that manages sexual and reproductive health programs to promote gender equality and safe access to reproductive services.
We Testify is a platform for individuals who have had abortions to tell their stories and experiences, creating better representation and visibility of abortions and those who receive them.
Who Not When is a people-centered resource for information and support on late-term abortions, and how abortion bans negatively impact reproductive health.
Women on Web is an international nonprofit that works to provide safe abortion pills in 200 countries via their online consultation.
Women’s Reproductive Rights Assistance Project is the largest independent nonprofit abortion in the United States, which provides financial assistance for abortion care and emergency contraception.
World Health Organization is the international authority on health research and best practices, which asserts that access to all healthcare (including sexual and reproductive healthcare) is a fundamental human right alongside the United Nations.
Young Women of Color 4 Reproductive Justice Collective is an Advocates for Youth program for women of color between the ages of 14 to 24, which aims to dismantle the discrimination and stigma young women of color experience while pursuing abortions.
Youth.GOV Adolescent Sexual Health is a government website that strengthens youth programs in the United States, which includes sexual health.